Lameness, foot abscesses and subtle neurological problems are the top performance and welfare disruptors in UK horses — and they’re far more common than many owners realise. With UK-specific data now consistent year-on-year, you can use proven benchmarks to spot issues sooner and manage them better.
Key takeaway: Lameness accounts for around 29% of all health problems reported in UK horses, with degenerative joint disease and foot problems (including abscesses) leading the way — so routine monitoring and fast, foot-first checks make the biggest difference.
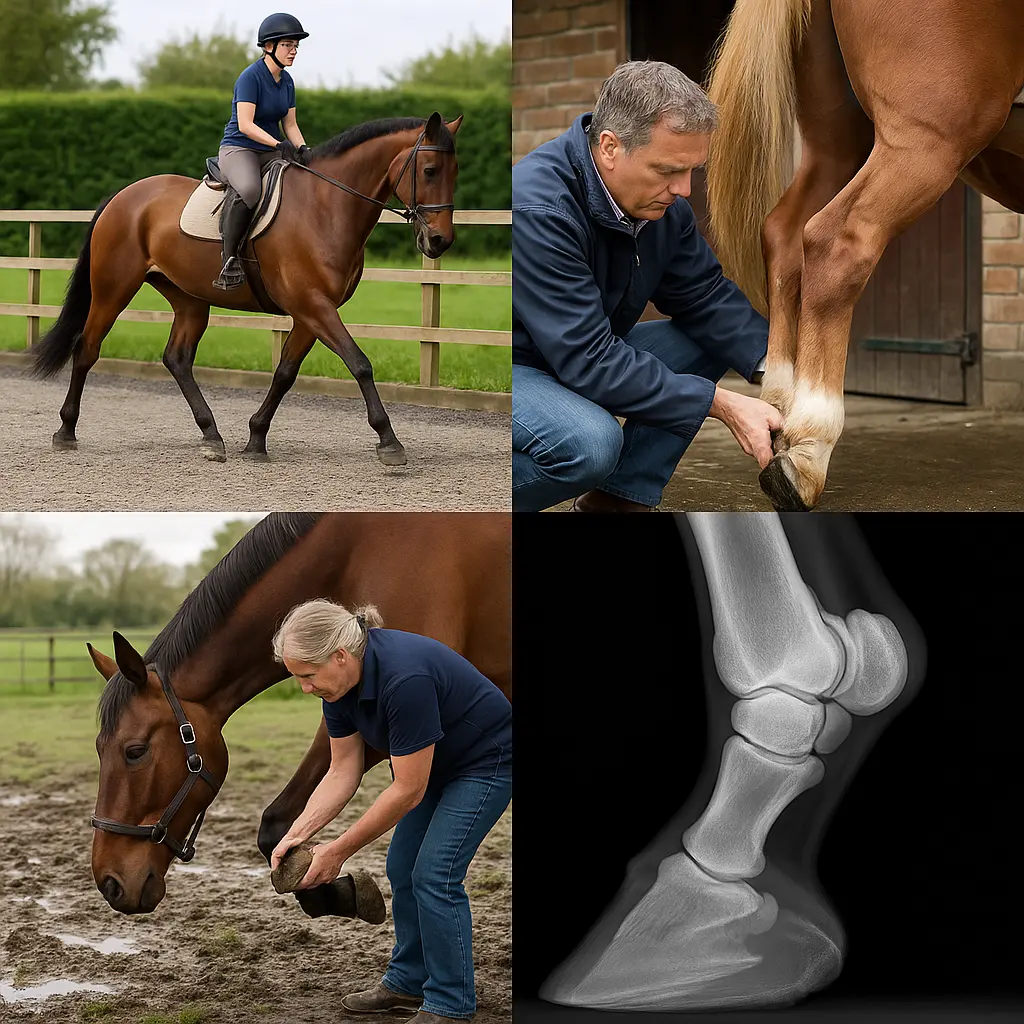
How common is lameness in UK horses?
Lameness represents approximately 29% of all health problems reported in UK horses, with around one-third of horses showing some degree of lameness at any time. These figures come from the National Equine Health Survey (NEHS), run by Blue Cross in partnership with BEVA, based on 16,751 horses reported by 5,635 participants.
Lameness consistently ranks as the second largest health category after skin disease in NEHS data, which BEVA and leading UK organisations consider a reliable national benchmark. That reliability matters: it lets you compare your yard’s experience with the wider UK picture and prioritise the checks that genuinely reduce risk.
“The year’s increase in overall lameness may be in part attributed to the higher incidence of pus in the foot but may also be because owners are becoming more aware of lameness issues… helping to raise understanding of the importance of accurate diagnosis and treatment both from welfare and performance perspectives.” — Josh Slater, Royal Veterinary College, BEVA Health & Medicines Committee, via Horse & Country
What causes most lameness—and what to watch for
Degenerative joint disease (DJD) is the single most common cause of lameness at 41.2% of cases, with the hock the joint most often affected, and nearly half of all lameness originates in the proximal limb rather than the foot. Foot problems still contribute substantially, with laminitis and non-laminitic foot lameness (including abscesses) together accounting for a large share of cases.
Breakdown highlights to guide your eye:
- Proximal limb lameness (above the foot) dominates: 47.4% of lameness. Expect subtle shortening of stride, difficulty stepping under, reluctance to canter or jump, or a “not quite right” feel on one rein.
- DJD patterns: 41.2% of lameness, commonly in the hock. Early signs include stiffness starting off, low-grade unevenness on circles, and reluctance in collected work.
- Laminitis: 18.4% of lameness. First and repeat episodes occur at similar rates (2.3% and 3.1%). Look for a pottery gait, heat in the feet, and sensitivity on hard ground.
- Other foot lameness: 13.7% of lameness and 4% of all syndromes; notably, foot lameness doubled between 2015 and 2016, with “pus in the foot” the most recorded cause. Expect sudden, often severe lameness in one limb, heat and a bounding digital pulse.
Quick tip: If you’re unsure where the lameness is coming from, start at the foot. It’s fast, objective (heat, pulse, hoof tester response), and covers a large chunk of real-world cases.
Foot lameness, laminitis and abscesses: spot the difference fast
You need a vet for a definitive diagnosis, but as a rule laminitis is a systemic, often bilateral foot problem, while abscesses (pus in the foot) cause sudden, severe, usually one-sided lameness; other foot soreness sits between these extremes. Knowing the presentation helps you act quickly and describe signs clearly to your vet and farrier.
What to look for at the yard:
- Abscess (pus in the foot): Typically acute, dramatic lameness in one leg; heat in the hoof, a strong digital pulse, possible focal reaction to hoof testers. UK wet winters and muddy gateways raise risk by softening soles and creating micro-cracks.
- Laminitis: Often affects both fronts; pottery, short steps, worse on hard ground, stance rocked back to unload the toes; may have heat and strong pulses in multiple feet.
- Other foot lameness (non-laminitic): Bruising, sole tenderness, nail bind, or mild infection can cause variable lameness that worsens on tight turns or hard surfaces.
Immediate actions that help:
- Call your vet and farrier early; coordinate so foot causes are ruled in or out promptly.
- Stable on a deep, supportive bed. For laminitis suspects, keep movement minimal until advised.
- If advised by your vet/farrier, poultice the foot and keep it clean and dry. Avoid pulling shoes or digging without guidance.
- Manage mud and wet. Regular hoof picking and dry standing areas reduce infection risk. Useful yard kit includes hoof picks, brushes and hoof care items from our hoof and grooming tools.
For turnout in relentless rain, keeping your horse comfortable and moving appropriately can help overall musculoskeletal health; browse well-fitting winter turnout rugs to balance protection with ventilation in changeable UK weather.

When to suspect neurological disease instead of lameness
Suspect a neurological issue when deficits don’t localise to a single limb, appear inconsistent, involve stumbling or toe-dragging, or affect all four limbs with poor coordination. Neurological problems can mimic lameness but won’t block to one leg and often worsen on tight turns, hills or with eyes covered.
Tell-tale patterns include:
- Ataxia (wobbliness), delayed placing of feet, crossing limbs, or inconsistent hind-end “lameness” that swaps legs.
- Toe-dragging marks in the school, scuffing on the dorsum of the hoof, or wearing the toes unevenly.
- Loss of balance when the tail is gently pulled sideways during walk, or marked deterioration on a tight circle or backing up.
If you see these signs, stop ridden work and call your vet promptly. Keep handling calm and safe. Once your vet sets a plan, ground-based rehab may include targeted, controlled exercise; fit-and-for-purpose support boots and bandages can help protect limbs during these sessions.
Monitor and document gait like a pro
Record short videos in straight lines and on circles on consistent surfaces, log dates and triggers, and compare every few weeks; regular, structured monitoring is the quickest path to early detection. Replicate the NEHS approach by keeping clear notes that transform “I think he’s off” into actionable data.
Set a simple baseline routine:
- Monthly check: Walk and trot up on a firm, level surface, both reins on the lunge, then under saddle if safe.
- Surfaces and speeds: Film on the same surfaces (hard/soft) and repeat gaits. Note any head-nod, hip hike, short stride or irregular rhythm.
- Triggers: Log shoeing dates, workload changes, turnout conditions (mud/dry), and any slip or knock.
- Rating scale: Use 0–5 for severity so changes are obvious over time.
Quick tip: Capture 10–15 second clips from front, behind and side. Many of our customers keep a shared phone album so your vet and farrier can review the same footage before a visit.
For comfort and protection during schooling and lunge work, choose appropriate support boots and bandages. If your vet confirms early DJD, consider adding targeted joint support supplements to your management plan.
Prevent and manage: daily routines that cut risk
Regular farrier care, footing and workload management, appropriate bodyweight, and routine veterinary checks are the most effective ways to reduce lameness risk. Coordinating between your farrier and vet ensures foot pathology is ruled out early before chasing higher-limb causes.
Build these habits into your yard calendar:
- Farrier first: Maintain a 5–7 week cycle. Discuss balance, breakover and sole depth, especially heading into wet months when abscess risk rises.
- Vet check-ins: Working horses benefit from periodic orthopaedic assessments, particularly hocks, given DJD’s 41.2% share of lameness and the hock’s leading involvement.
- Surface sense: Vary footing to avoid repetitive strain; keep arenas maintained and avoid deep, shifting surfaces that stress proximal structures.
- Weight and workload: Gradual increases, active warm-ups, and cool-downs protect joints, tendons and ligaments.
- Mud management: Gateways and tracks with hardcore, regular hoof picking, and dry standing areas reduce foot infections.
- Record-keeping: Mirror NEHS-style notes — episode dates, duration, and potential triggers — to spot patterns you’d otherwise miss.
At Just Horse Riders, we recommend a “comfort kit” for the wettest weeks: weather-ready turnout rugs for the field, cosy stable rugs for recovery, and targeted joint support supplements for horses increasing their workload or showing mild age-related stiffness. Popular choices include trusted formulas from NAF joint and hoof supplements.
Eventers and competition horses: raise your game
Eventing horses report the highest musculoskeletal problem rates — 49.4% with previous issues and 26% experiencing episodes in the prior six months — so they need stricter monitoring and longer recovery windows. Most issues cluster in the foot, joints, back, ligaments and tendons, reflecting the demands of training and competition.
Practical upgrades for competition yards:
- Structured week: Alternate high-impact sessions with technique or hack days; always include thorough warm-ups and cool-downs.
- Hoof vigilance: Daily checks pre- and post-work; prompt attention to any heat or digital pulse change, especially after hard or muddy going.
- Joint management: Early veterinary input for any recurring “off” days; baseline hock assessments help you act before a blip becomes a breakdown.
- Protection: Choose quality boots for gallops and jumping, and consider bandaging for travel and recovery. Explore performance-led ranges from LeMieux boots and pads.
- Evidence bank: Keep competition clips and schooling videos; annotate with footing, speed, and feel to help your vet pinpoint patterns.
What to do today if your horse looks ‘not quite right’
Start with a calm, methodical foot-first check, film a straight-line trot-up and circles, and call your farrier and vet with your findings; early, coordinated action saves time, money and discomfort. Most “NQR” horses fit within the big UK patterns: foot, hock/DJD, or proximal soft tissue — so your initial steps should rule these in or out quickly.
- Check feet: Heat, digital pulse, hoof cracks, sole bruising, lost or tight nails. If acutely lame, stable on a deep bed and call your vet/farrier.
- Film and log: Front/side/behind on firm ground; note surface, gait, tack and any recent changes (shoeing, workload, mud).
- Feel joints and back: Note localised heat or swelling; mild hock stiffness after rest suggests early DJD — speak to your vet about assessment.
- Decide safe exercise: If mild and improving, stick to straight lines on consistent footing; avoid small circles until you have guidance.
- Support recovery: For controlled exercise, use well-fitted support boots and bandages. Review turnout and bedding to keep feet clean and dry.
Pro tip: Book your farrier and vet back-to-back when possible. Many cases shortcut to the answer when both see the horse on the same day.
Quick tip: If signs suggest a neurological problem (wobbliness, toe-dragging both sides, stumbling), stop ridden work immediately and call your vet.
Used together — clear videos, good notes and rapid foot checks — these steps mirror the data-driven approach behind BEVA-supported NEHS figures and lead to faster, more accurate diagnoses.
FAQs
How common is lameness in UK horses?
Lameness accounts for about 29% of all health problems reported, and roughly one in three horses shows some degree of lameness. NEHS data, supported by BEVA and Blue Cross, provides the national benchmark for these figures.
What’s the most common cause of lameness?
Degenerative joint disease (DJD) is the leading single cause at 41.2% of lameness cases, with the hock being the joint most frequently involved.
How do I tell laminitis from an abscess?
Laminitis often affects both front feet with a pottery gait and is worse on hard ground, while an abscess (pus in the foot) typically causes sudden, severe lameness in one limb with heat and a strong digital pulse. Your vet and farrier will confirm and advise treatment.
Are foot problems really that common?
Yes. Non-laminitic foot lameness accounts for 13.7% of lameness cases and 4% of all syndromes; it doubled between 2015 and 2016, with abscesses the most frequently recorded foot issue.
How often should I have my horse assessed for lameness?
Working horses benefit from periodic veterinary orthopaedic assessments, particularly of the hocks, and immediate checks if you notice changes. Eventers are high risk, with 26% reporting musculoskeletal episodes in the previous six months.
When should I suspect a neurological problem?
Consider neurology if deficits don’t localise to one limb, you see toe-dragging or stumbling, signs shift between legs, or coordination worsens on tight circles or with eyes covered. Stop ridden work and call your vet promptly.
What products help me manage and monitor issues?
Keep a tidy hoof-care routine with our hoof and grooming tools, protect limbs during controlled exercise with support boots and bandages, manage weather with turnout rugs and stable rugs, and support joints with targeted joint supplements including options from NAF.