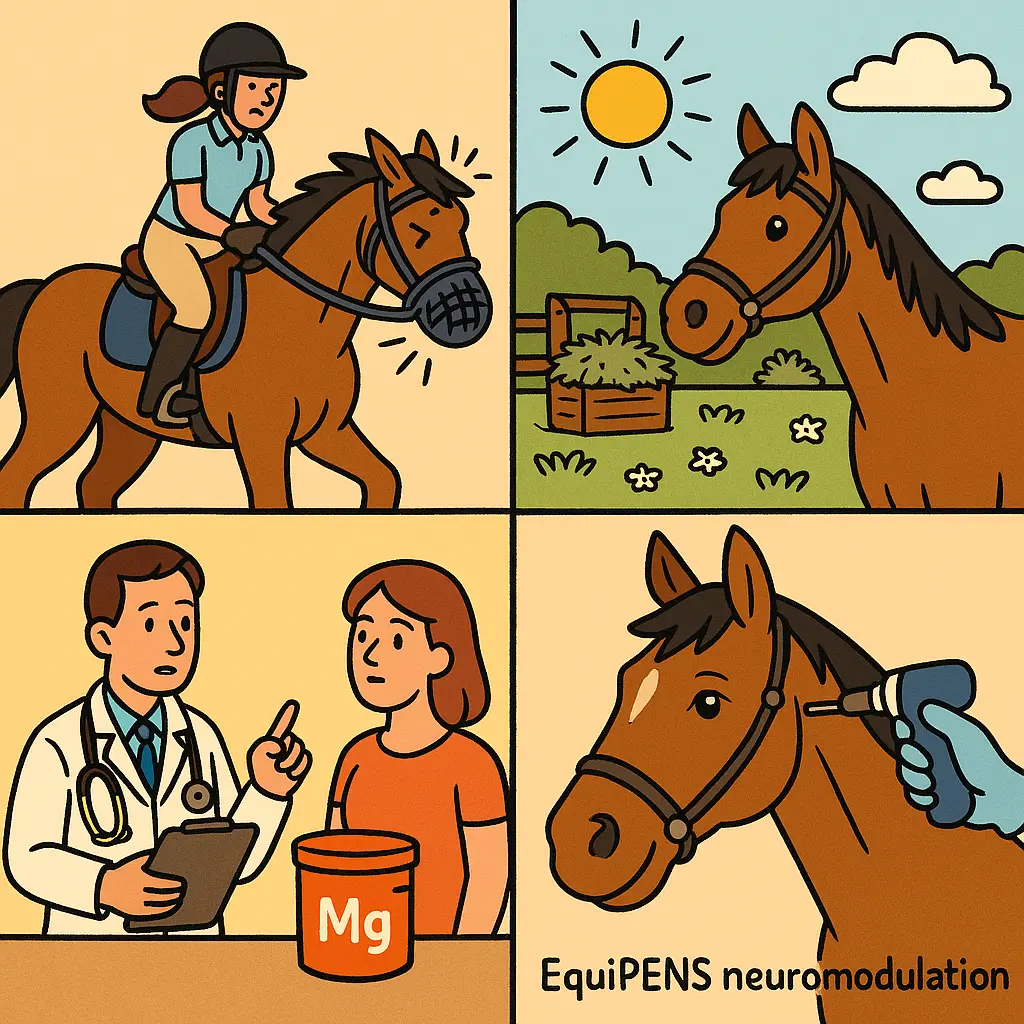
If your horse is flicking, snorting, or violently tossing his head—especially in spring and summer—you’re not alone. Trigeminal-mediated headshaking affects up to 1–4.6% of horses in the UK, with geldings over-represented and signs often worse in bright, warm weather.
Key takeaway: Magnesium can reduce headshaking signs by around 29–64% depending on the form and route, but it doesn’t cure the condition—use it as part of a vet-led, holistic plan that also tackles light, pollen, and pain triggers.
What is trigeminal-mediated headshaking?
Trigeminal-mediated headshaking is a neuropathic pain syndrome where the trigeminal nerve becomes hypersensitive, causing abrupt head flicks, snorting, rubbing, and striking at the face, often worse in trot and canter. Between 1% and 4.6% of horses are affected, around 75% are geldings, and signs frequently peak in UK spring/summer.
Owners commonly report seasonal flares linked to brighter light and higher pollen counts, with some horses markedly better in winter or at night. Many headshakers rub their muzzle on legs or the ground and become difficult to ride, with safety concerns escalating at faster gaits where the trigeminal nerve is further stimulated.
Despite the welfare and safety impact, only 25% of affected horses see a vet, while 84% of owners try alternative therapies and just 11% opt for scientifically tested treatments. Be in the 25%: a BEVA-registered vet can help confirm the diagnosis, rule out dental, sinus, ocular, or tack issues, and build a treatment plan.
Does magnesium help headshaking?
Yes—magnesium can reduce headshaking signs, with intravenous magnesium sulphate decreasing behaviours by about 29% and oral magnesium citrate (when paired with boron in research) showing around 64% reductions in walk and canter assessments. It does not cure headshaking and should be combined with management and other treatments.
Magnesium is thought to calm overactive nerve firing, making it a rational adjunct in trigeminal hypersensitivity. In studies, IV magnesium sulphate produced peak effects 30–120 minutes post-infusion and improvements lasted roughly two hours. Oral magnesium citrate plus boron achieved larger reductions, but adding boron is not permitted in UK horse feeds, so UK owners should focus on well-absorbed magnesium citrate alone under veterinary guidance.
“Magnesium sulphate intravenously decreased headshaking by 29%. Magnesium citrate and boron orally decreased headshaking by 64%... Moderate owner expectations to a slight reduction in signs, but to be used as part of a holistic approach.” — Vet Times
Anecdotally, some owners report around a 40% decrease with oral magnesium sulphate, but absorption varies by form. UK specialists commonly prefer magnesium citrate because it is more readily absorbed than some other salts.
“We recommend giving a magnesium supplement alongside [EquiPENS]. There is evidence that magnesium citrate is more easily absorbed than other types.” — B&W Equine Vets
Bottom line: magnesium can help, but expect partial improvement. Use it alongside nose nets, dietary changes, and, where appropriate, neuromodulation techniques such as EquiPENS.
How to trial magnesium safely in the UK
Always involve your vet before starting magnesium, test blood magnesium first, and avoid total magnesium values above 2 mg/dL to reduce the risk of side effects. No UK labs routinely measure ionised magnesium, so vets use total magnesium and established calculations (e.g., Marlin, 2023) to guide dosing and monitoring.
Because headshaking often escalates in trot and canter, your vet may suggest a controlled ridden assessment to baseline your horse’s signs before starting. If a rapid, short-term “test” is needed, your vet can trial an intravenous magnesium sulphate infusion and you can expect a 29–51% reduction in headshakes for roughly two hours; if your horse responds, an oral trial may be worthwhile.
For oral supplementation, choose UK-legal magnesium citrate products without boron, start low, and build gradually while your vet tracks clinical response and serum magnesium. Reassess at four weeks: if there’s no clear improvement, stop to avoid unnecessary supplementation and potential toxicity.
Signs of excessive magnesium include sweating, weakness, agitation, irregular heart rate, and respiratory problems—seek immediate veterinary advice if these occur. Remember that diet, workload, and weather all influence nerve excitability, so magnesium should sit inside a broader plan rather than be relied upon in isolation.
Pro tip: Keep a simple log of ridden sessions and signs (frequency of flicks per minute in walk/trot/canter). This makes it easier for your vet to interpret whether magnesium is genuinely helping.

Build a holistic plan: management that actually helps
The most effective approach combines magnesium with nose nets, light and pollen management, and diet tailored away from high-potassium ryegrass. This “stacking” of small wins often outperforms any single intervention.
Practical steps UK owners find useful include:
- Use a well-fitted nose net during ridden work to reduce facial irritation and airflow triggers. Many horses show immediate improvement with this low-cost measure.
- Ride at times of lower light intensity (early morning/evening) and avoid strong headwinds that intensify nasal stimulation.
- Manage flies and midges in warm months with masks and fly rugs; consider breathable summer fly rugs to limit insect contact over sensitive areas.
- Feed meadow or timothy hay/haylage rather than ryegrass where possible, and avoid lush, high-potassium spring grass. Some horses cope better on balanced concentrates than on hay-only diets.
- Keep the muzzle clean and dry—dust, pollen, or sweat can irritate. A soft grooming kit used before you tack up can make a difference.
- If your horse strikes at his face with a foreleg, protect limbs to prevent knocks and abrasions using well-fitted protective horse boots.
At Just Horse Riders, we recommend tackling management methodically: add one change at a time, measure its impact, and keep what works. This avoids confusion and helps your vet refine the plan.
When magnesium isn’t enough: EquiPENS and vet-led options
EquiPENS neuromodulation delivers 50–53% initial remission rates across large UK case series, with a median remission time of around 9.5 weeks after the first set of procedures. It’s widely available through UK equine hospitals and is a logical next step if nose nets and magnesium don’t deliver safe, rideable results.
EquiPENS involves percutaneous electrical nerve stimulation across the trigeminal distribution. Typically, three procedures are performed initially; many responders then need periodic top-ups. UK vets such as the B&W Equine Vets team offer EquiPENS and actively recommend pairing it with magnesium citrate to support nerve stability.
“We recommend giving a magnesium supplement alongside [EquiPENS].” — B&W Equine Vets
For non-responders, your vet may discuss diagnostic nerve blocks or other targeted therapies. Keep expectations realistic: while about half achieve remission with EquiPENS, others see partial improvement that still meaningfully improves safety and comfort. Continue your management stack—nose nets, seasonal timing, diet, and magnesium—to maximise the benefit.
Quick tip: Book EquiPENS well before peak season. Many UK horses worsen sharply from April to August; proactive scheduling helps you get ahead of pollen and light triggers.
Feeding and kit: UK-legal products that support headshakers
Choose magnesium citrate-only supplements (without boron) and reassess effect within four weeks while your vet monitors serum levels. Boron is not licensed for inclusion in UK equine feeds, so do not add it to pursue the higher reductions seen in US studies.
Look for reputable manufacturers and clear labelling, and avoid stacking multiple products that may duplicate magnesium. A single, well-formulated product is safer and easier to evaluate. You can find a wide range of reputable options in our curated magnesium and nerve-support supplements collection, and we also carry electrolyte balancers—useful if your horse is sweating more in warmer months—which are available from trusted brands such as NAF.
Kit that often helps day-to-day includes:
- Nose nets and fly masks to shield the muzzle from airflow, dust, and insects. Explore proven designs from brands like WeatherBeeta and Shires.
- Summer protection that stays breathable—our selection of fly rugs supports horses that are particularly sensitive in warm, bright conditions.
- Gentle facial grooming tools—see our grooming essentials—to remove dust and pollen before riding without aggravating sensitive skin.
- Safety kit for you: a well-fitted riding helmet and hi-vis are sensible if your horse can be unpredictable; browse our rider ranges if needed.
Our customers often report that small upgrades to fit and comfort—like softer noseband padding or reducing bridle weight—lower irritation. While these don’t treat the nerve itself, they can reduce additional triggers that tip a borderline ride into a difficult one.
Your step-by-step action plan
Act early, act methodically, and measure what matters. Here’s a UK-focused plan you can start this week:
- Book a vet exam. Ask specifically about trigeminal-mediated headshaking and request a structured ridden assessment in walk/trot/canter to baseline signs.
- Rule out and address other causes. Your vet will consider dental disease, bit/bridle fit, sinus or ocular problems, and pain elsewhere.
- Start management now. Add a nose net, adjust ride times to early/late to avoid glare, reduce headwinds on hacks, and switch to meadow/timothy hay/haylage if you can. Use a gentle grooming kit to clear pollen before riding.
- Discuss a magnesium plan. Test blood magnesium first. If appropriate, start a magnesium citrate-only supplement and reassess at four weeks, tracking signs by gait.
- Consider an IV magnesium “test.” Under vet supervision, a single infusion can predict whether your horse is a magnesium responder (expect 29–51% reduction for about two hours if effective).
- Stack summer protection. Add a breathable fly rug and well-fitted fly mask; consider leg protection with horse boots if your horse strikes at the face.
- Escalate if needed. If magnesium plus management isn’t enough, plan EquiPENS with your vet—initial remission runs around 50–53% with a median of 9.5 weeks.
- Review and refine. Keep what works, cull what doesn’t. Re-test serum magnesium to stay safely below 2 mg/dL and watch for side effects (sweating, weakness, agitation, arrhythmias, breathing issues).
At Just Horse Riders, we’re here to help you put the practical pieces in place—from nose nets and fly rugs to carefully selected supplements—while your vet leads on diagnosis and medical treatment.
FAQs
Does magnesium cure headshaking?
No. Magnesium reduces signs but doesn’t cure the neuropathic pain. IV magnesium sulphate reduced headshaking by about 29% for up to two hours, and oral magnesium citrate with boron achieved around 64% in research settings. In the UK, use citrate-only products alongside wider management and vet-led care.
Is adding boron safe or legal in the UK?
No. Boron is not permitted in UK horse feeds, so don’t attempt to replicate overseas magnesium–boron protocols. Choose magnesium citrate-only products and work with your vet.
When does magnesium backfire?
Excess magnesium can cause sweating, weakness, agitation, irregular heart rate, and breathing problems, particularly if total serum magnesium exceeds 2 mg/dL. Always test before and during supplementation and stop if adverse signs appear.
How seasonal is headshaking?
Very often seasonal in the UK—most cases worsen in spring and summer with brighter light, higher pollen, and warmer, windier rides. Around 75% of affected horses are geldings.
How does EquiPENS compare with magnesium?
Magnesium typically offers slight-to-moderate reductions in signs. EquiPENS achieves remission rates of about 50–53% after initial procedures, with a median remission of 9.5 weeks. Many owners use both: magnesium for nerve-calming plus EquiPENS for neuromodulation.
Can I try magnesium without seeing a vet?
No. Only a quarter of headshaking horses see a vet, yet unmonitored supplementation risks toxicity and delays effective treatment. Start with a veterinary examination and blood testing, then build a monitored plan.
Which magnesium form is best?
UK vets commonly recommend magnesium citrate because it’s more easily absorbed than some other forms. Choose UK-legal products without boron, start low, and reassess at four weeks.
Further reading and expert guidance: Vet Times – latest research summary, B&W Equine Vets – UK treatment options including EquiPENS, and Science Supplements – magnesium overview. At Just Horse Riders, we stock the practical tools—nose nets, masks, fly rugs, and carefully selected supplements—to support the plan you craft with your vet.



